Imported spices and frozen vegetables tested for “superbugs”
A University of Saskatchewan research team has found that some food imported to Saskatoon from certain Asian countries has tested positive for “superbugs”—strains of antibiotic-resistant bacteria— but immediate health concerns are likely low.
By Federica GiannelliA University of Saskatchewan research team has found that some food imported to Saskatoon from certain Asian countries has tested positive for “superbugs”—strains of antibiotic-resistant bacteria— but immediate health concerns are likely low.
“Our study is among the first in Canada to look at antimicrobial resistance in imported plant-based products, and we hope our research will help expand the monitoring of antimicrobial resistance transmission to these foods which are currently not included in the national surveillance programs,” said Dr. Joe Rubin, a professor in the Western College of Veterinary Medicine’s department of veterinary microbiology.
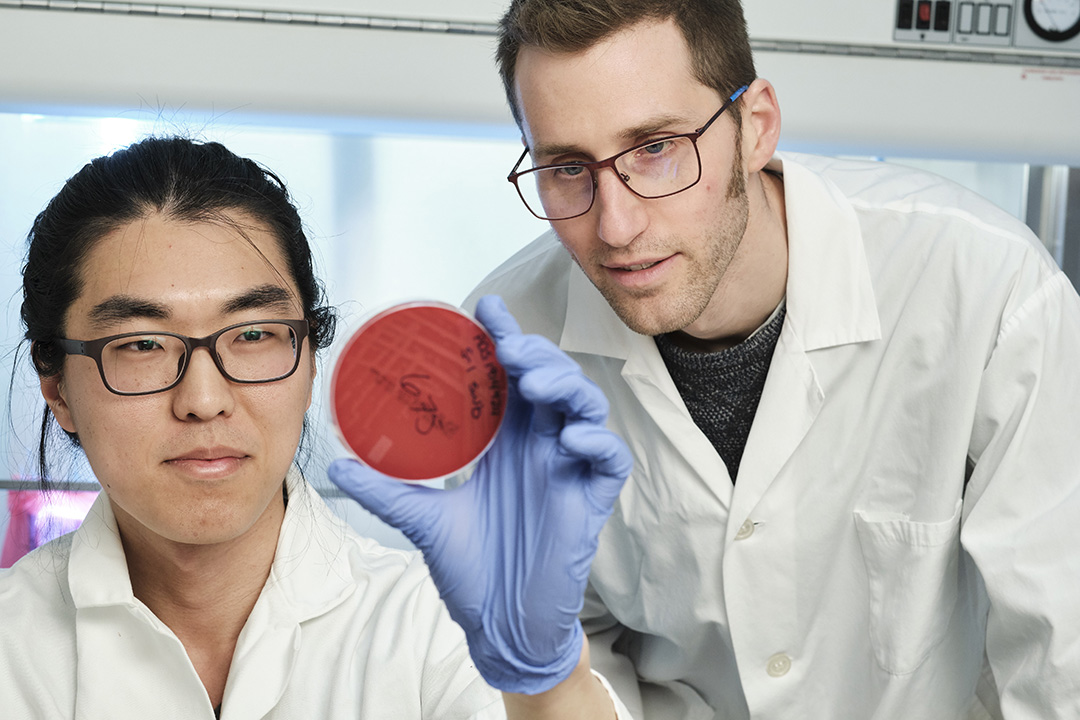
Rubin and his recently graduated master’s student Dongyun Jung have analyzed almost 150 samples of spices, frozen vegetables and dry food including beans and seeds purchased in small shops which sell imported food.
The researchers found “superbugs” in eight samples—about five per cent of the products tested: E. coli; Klebsiella pneumoniae (a type of bacteria causing pneumonia); some species of Enterobacter and Enterococcus; Staphylococcus aureus and MRSA (Methicillin-resistant Staphylococcus aureus). All of these are versions of the bacteria resistant to antibiotics, and resistance may cause treatment failure or make infections more difficult to treat.
The food analyzed came from regions of the world where antibiotic resistance is more common, but Rubin said the bacterial contaminations may happen anywhere in the shipping and retail process, in Canada or abroad. He plans to expand his research to look at the extent to which “superbugs” are present in domestic food, so that comparisons with imported food can be made.
“Our goal is to show whether these bacteria might move from countries with high prevalence of these ‘superbugs’ to countries with low prevalence such as Canada via imported foods, and to show whether these bacteria contain antibiotic resistance genes that can be transmitted to other susceptible bacteria,” said Jung, a South Korean student.
The results of this project, funded by the federal agency NSERC, have been presented at national and international conferences.
Rubin said that the reason we are not hearing about people getting sick or dying is that the concentration of bacteria in food items varies greatly and is often low. Depending on the type of bacteria, infections only occur when people are exposed to large quantities of pathogen, and when the acids in the gut fail to kill the bacteria ingested.
“Bacteria live around us. We don’t live in a sterile environment—we shouldn’t—and food is never sterile, so eating a single item where these bacteria are present doesn’t make you sick in most cases,” said Rubin.
Canada’s antimicrobial resistance surveillance system called CIPARS monitors antibiotic resistance in human, animal and food sources, but the program focuses on meat-derived products.
Rubin stresses that potential exposure to food-borne bacteria can be avoided by keeping kitchen surfaces and tools clean, separating raw and cooked food, cooking food thoroughly at high temperatures, which kills bacteria, and keeping food at safe temperatures.
He hopes to study the impact of human exposure to food contaminated with “superbugs,” that can transmit antibiotic-resistant genes to other bacteria innocuously living in our body and make treatment of future infections more difficult.
While bacteria slowly adapt to the drugs used to treat infections over time, the misuse and overuse of antibiotics in humans and animals, as well as poor infection prevention and control, have contributed to the emergence of antibiotic resistance. A 2016 UK major study estimates that costs will be $40 billion U.S. over a decade to take global action against “superbugs.”
Federica Giannelli is a graduate student intern in the University of Saskatchewan research profile and impact unit. This article first ran as part of the 2019 Young Innovators series, an initiative of the USask Research Profile and Impact office in partnership with the Saskatoon StarPhoenix.”
