Therapy may reduce muscle atrophy in spinal cord injury patients
A team of researchers at the University of Saskatchewan (USask) is investigating a therapy for spinal cord injuries that could potentially increase patients’ motor function and decrease muscle atrophy at the same time.
By Rachel McCannAcute intermittent hypoxia (AIH) therapy exposes patients with spinal cord injuries (SCI) to short periods of low or hypoxic oxygen levels (11 per cent) alternated with periods of normal oxygen levels (21 per cent).
This fluctuating exposure triggers a chain of events in the nerve cells or neurons as they react to the mild stress. Over time, this reactive response in the nervous system promotes changes that improve a patient’s recovery of motor function, including increased strength in the limbs and more efficient movement.
“Acute intermittent hypoxia is a really great treatment option because it’s non-invasive,” says Dr. Breanna Arnold, a PhD candidate in the Western College of Veterinary Medicine’s (WCVM) Department of Veterinary Biomedical Sciences. “With AIH, all you have to do is breathe in a lowered level of oxygen, so it is very non-invasive, very safe and effective as well.”
Specifically, the therapy appears to enhance neural plasticity, whereby the nervous system responds to damage to pathways by establishing new routes or networks of communication.
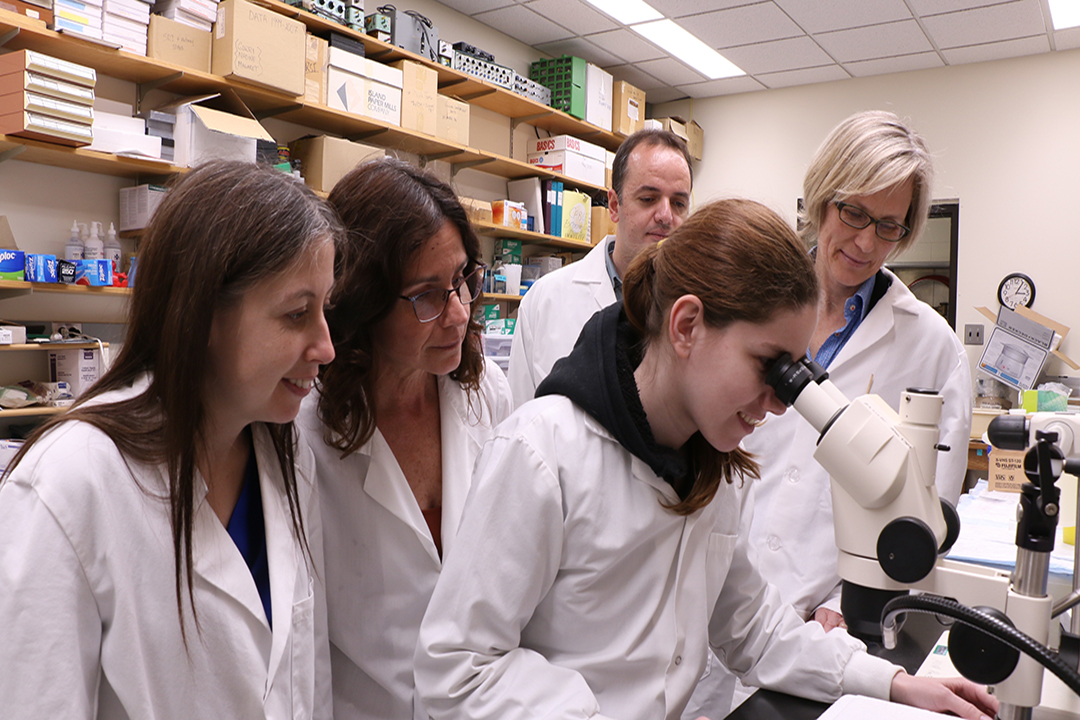
Arnold is part of a multi-disciplinary research team led by WCVM professor Dr. Gillian Muir and Dr. Valerie Verge, a professor of anatomy and cell biology at the USask College of Medicine. The AIH research work has financial support from the Saskatchewan Health Reseach Foundation, Canadian Institutes of Health Research and the United States Department of Defense.
Muir leads this particular study in which laboratory rats with SCI were trained to perform various motor tasks that demonstrated their motor function and recovery. The researchers were able to confirm the value of AIH therapy by showing that animals treated with AIH had improved motor recovery.
While observing AIH therapy’s positive impact on the motor capabilities of the laboratory animals, the scientists began to suspect that these improvements might be not only due to neural plasticity but also to changes in muscle tissue — an exciting concept that takes AIH treatment to another new level of investigation.
Spinal cord injuries are known to cause muscle degradation or atrophy — the result of both neuron damage and the lack of use of the muscle. In order to maintain adequate muscle tissue, the rate of muscle metabolism needs to be high enough that new proteins are being built (protein synthesis) faster than they break down (protein degradation).
“After SCI, there are changes in muscle function and also there is atrophy of the muscles,” explains Dr. Behzad Toosi, a research associate at the WCVM who participated in the study. “The thing that makes it complicated in terms of recovery for patients after SCI is the muscle atrophy, especially because it starts early after the injury.”
While the mechanisms are not completely known, the problem is an imbalance in protein synthesis versus protein degradation, adds Toosi.
“After SCI, we have more protein degradation compared to protein synthesis, and that causes a loss in muscle volume, muscle endurance, and power or strength.”
Since muscle is a very important tissue for metabolism within the body, the SCI patients don’t just experience problems with movement; they also run the risk of developing secondary diseases, including diabetes and heart disease.
If AIH can somehow reduce muscle atrophy, it may significantly reduce the SCI patients’ risk of developing these secondary diseases.
While Muir and her team are encouraged by their results and the positive effects of AIH on motor recovery, they’re also excited at the prospect of investigating the impact of AIH on muscle atrophy.
Toosi is optimistic that their diverse approach to the uses for AIH could translate into new procedures in clinics that will benefit patients and enhance their recovery from spinal cord injuries. Human pre-clinical trials using AIH have already been carried out with promising results that including increased walking speeds and endurance in patients with spinal cord injuries.
“We are very focused on the effects of AIH on neural plasticity and improving the function of the motor neurons … and the results are very promising,” says Toosi.
“However, to put this in a big package to investigate the effects of AIH on neuronal function as well as muscle function and neuronal-muscle interaction … could provide some valuable clues for us; for example, how to adjust our AIH treatments in order to get optimal effects on motor recovery in terms of both neural plasticity and muscle function.”
Rachel McCann of Beaumont, Alta., will begin her third year of veterinary studies at the WCVM in August 2019. Her story is part of a series of articles written by WCVM summer research students.
