
Cancer therapies connect dogs and people
Dogs may hold the key to uncovering novel cancer therapy targets and treatments that will benefit domestic animals and their owners, as well as human cancer patients.
By Velina Milkova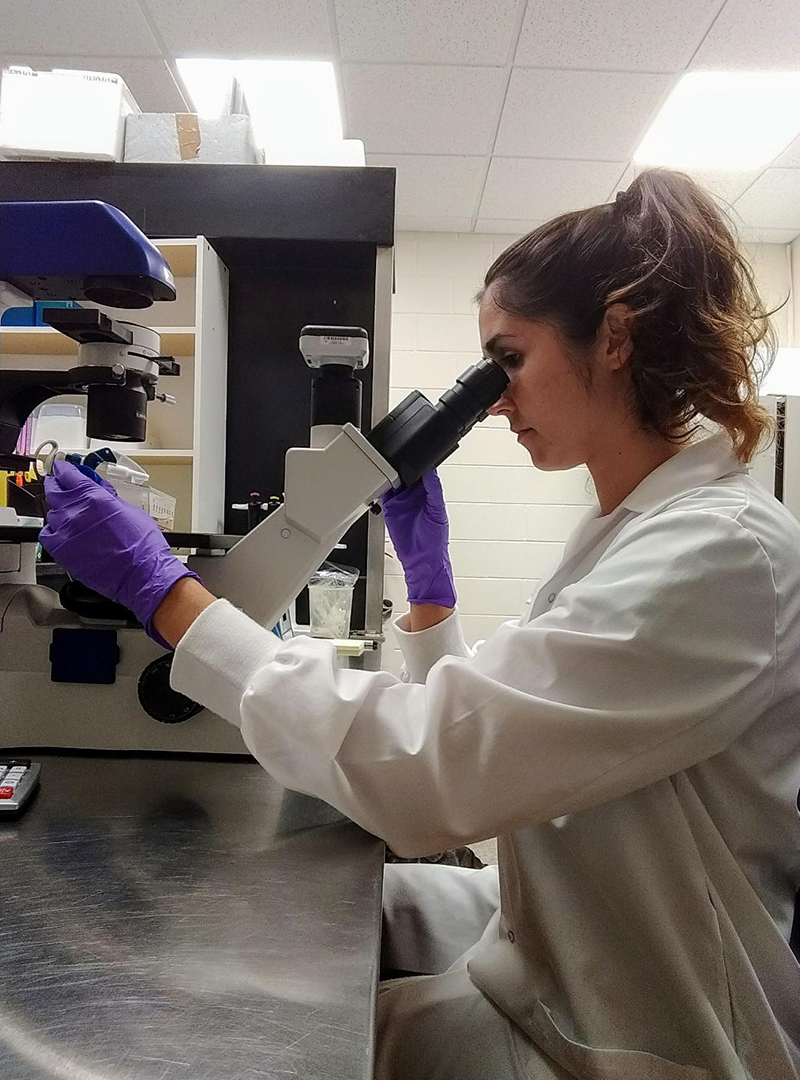
“Testing of new therapies in animals with naturally occurring tumours that are similar to those of humans has the capacity to reduce the time for clinical development of new pharmaceutical agents for human cancer therapy,” said Dr. Behzad Toosi (DVM), an assistant professor in the Department of Small Animal Clinical Sciences at the Western College of Veterinary Medicine (WCVM).
“At the same time, this provides an opportunity to bring the novel and advanced diagnostics and therapeutics from human drug discovery research to veterinary medicine.”
Research has shown that dogs develop similar cancers to people in terms of appearance, genetics and response to treatment. Since cancers in dogs and humans arise in similar environmental conditions, researchers can use canine cancer tumours to better understand human tumour progression.
These findings support the emergence of comparative oncology, which integrates human and veterinary medicine by studying canine tumours as models for human cancers.
As part of the University of Saskatchewan’s (USask) Comparative Oncology Research Group, Toosi’s research team is investigating a molecular similarity that could exist in canine and human cancers of the bone, mammary gland, lymphocytes and blood cells.
Researchers have previously shown that a group of cell surface proteins, called Eph receptor tyrosine kinases, are involved in multiple human cancers—making them potential targets for therapy.
“Protein kinases such as Eph receptor tyrosine kinases are important molecules in the context of cancer research as they drive various cancer properties,” said Toosi, who also holds the WCVM’s Allard Research Chair in Oncology.
“We strongly hope that [our research] goals will facilitate development of more effective cancer therapies that could be used for both companion animals and humans.”
Although these receptors have been studied in human cancers, no other research lab has evaluated their involvement in canine malignancies. In addition, existing research has targeted only a few of the many Eph receptor subtypes that are naturally found in non-cancerous cells.
Toosi is hopeful their research will reveal that these unexplored targets are similarly expressed in canine tumours—a finding that would open the door to developing new anti-cancer drugs that could be used to treat canine patients.
Developing and testing drugs and novel therapies on canine models before adapting them to human medicine has many advantages. Primarily, it helps to accelerate drug testing and approval. While human medicine has strict guidelines on clinical trials, veterinary medicine has a much faster approval process that still adheres to ethical guidelines.

Since dogs’ life cycles are shorter than those of people and their cancers progress more quickly, results from clinical drug trials are also accessible more quickly than they would be in human trials. Both animal and human patients benefit from the wider array of treatments and drugs that can be made available in this shorter time frame.
Given the multitude of similarities between canine and human malignancies, the best approach for cancer research is comparative oncology—a field that combines the efforts of veterinary and human medical professionals to bridge the gap between human and animal health.
Oncology research conducted by Toosi’s team has received financial support from the Allard Research Chair, WCVM, and the Saskatchewan Health Research Foundation.
Velina Milkova of Victoria, B.C., is a third-year veterinary student at the USask Western College of Veterinary Medicine (WCVM).
