Breathing new life: harnessing hypoxia to heal spinal cord injuries
University of Saskatchewan scientists are studying how therapeutic acute intermittent hypoxia (tAIH) works to promote spinal cord plasticity after an injury and identifying molecules and pathways activated by tAIH.
By Emily YauDon’t hold your breath for a treatment for spinal cord injury — or maybe do.
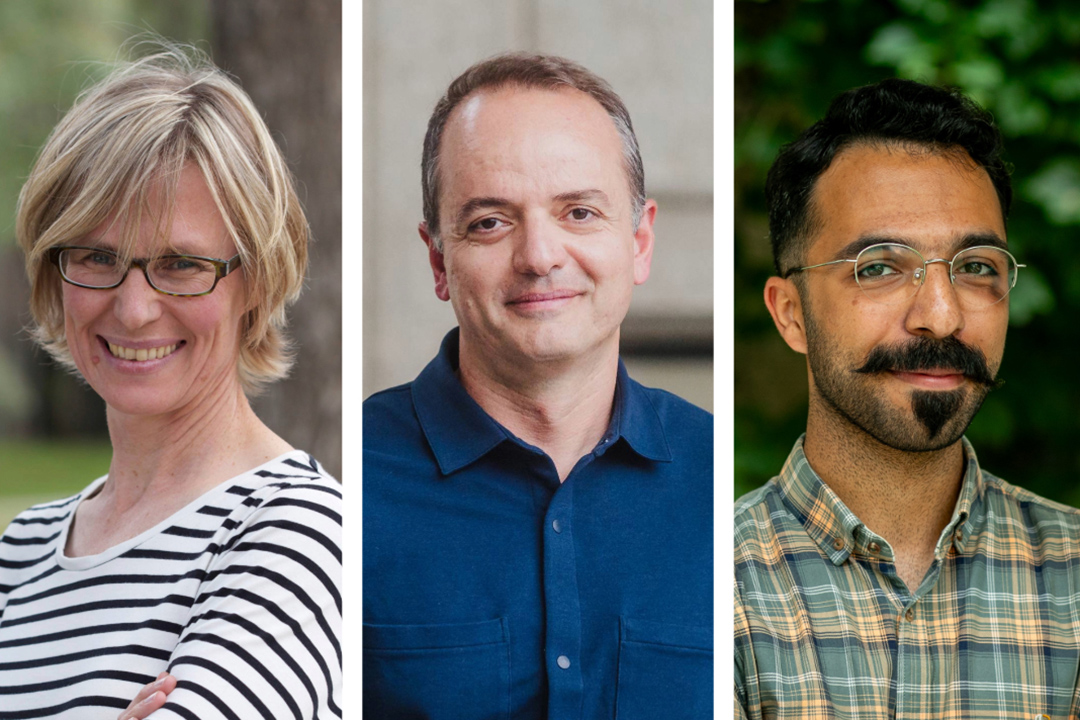
University of Saskatchewan scientists Drs. Gillian Muir (DVM, PhD) and Behzad Toosi (DVM, PhD), along with their research team at the Western College of Veterinary Medicine (WCVM), are investigating how therapeutic acute intermittent hypoxia (tAIH) works to promote spinal cord plasticity after an injury and could lead to promising targets for future therapies.
The impact of spinal cord injuries
A spinal cord injury (SCI) can alter a person’s life in an instant. The unpredictable nature of how these injuries come to be — motor vehicle accidents, a rough tumble in football, a poorly timed turn on a bicycle — puts anyone at risk. These injuries can have a profound impact on individuals from all walks of life, reaching beyond physical limitations to negatively affect autonomy, independence and overall quality of life.
Currently, there is no established and well-understood treatment for SCI. Therapeutic acute intermittent hypoxia (tAIH) has been shown experimentally to produce some improvement in motor function when applied to people with spinal cord injuries. However, the underlying mechanism of how tAIH works remains unclear.
Understanding the role of tAIH in spinal cord injuries
For decades, Muir has been investigating the recovery of key behaviours — including locomotion and reach-to-grasp ability — following SCI in rodent models.
“For people with SCI who are confined to a wheelchair, their ability to reach out and grab an object really determines how much they can do for themselves and live independently. To be able to provide a therapy that improves that function would really help people with SCI,” explains Muir, a neuroscientist and dean of the WCVM.
tAIH exposes tissues to brief periods of low oxygen levels. This experimental treatment has shown promise in enhancing cellular plasticity, which refers to the ability of cells (including neurons in the spinal cord) to adapt and reorganize. This ability is crucial for recovery and regeneration following injury.
But how can limiting a person’s oxygen levels be a good thing?
“Certainly, hypoxia can be a bad thing. When people have sleep apnea, for example, they experience intermittent hypoxia which can be quite severe, and over the long term, is physiologically harmful,” says Muir.
“The kind of hypoxia used in tAIH is a brief exposure to mild hypoxia … similar to the level of hypoxia [that] athletes use to improve plasticity in their muscle cells. In this case, the hypoxia activates molecules and pathways that improves athletic performance.”
However, tAIH alone is not the answer.
“tAIH enhances the capacity for plasticity in the spinal cord and brain, but you also need rehabilitation training to actually produce sustained changes in the neural pathways responsible for recovery. The movements you are making during training, such as reach-to-grasp movements, will strengthen the neural connections involved in grasping so that the function gradually improves. It’s hypoxia combined with rehabilitation training that produces the recovery effect we see,” Muir explains.
The work continues
In recent years, Dr. Behzad Toosi has joined forces with Muir to improve outcomes for people with SCI. Toosi is an assistant professor at the WCVM who also holds the college’s Allard Research Chair in Oncology. His current research work builds on Muir’s past studies, focusing on the molecular basis of spinal cord plasticity.
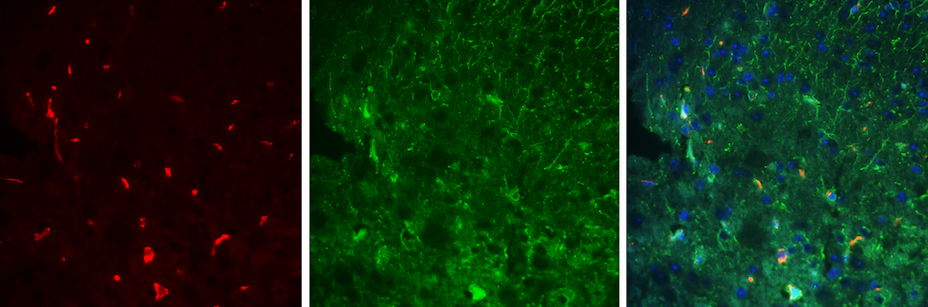
This summer, Toosi and his graduate student, Dr. Nima Khalili Tanha (DVM), are investigating the recovery of locomotion and grasping ability in mice by observing their ability to traverse a narrow beam while receiving tAIH. They aim to identify key molecules and pathways activated by tAIH to understand how this treatment works. To achieve this, they’re analyzing spinal cord tissue from mice using a variety of chemical techniques.
By identifying molecules and pathways activated by tAIH within injured spinal cords, the team hopes to contribute to the development of targeted therapies revolutionizing SCI treatment, offering hope to people with these life-altering injuries.
The future of tAIH research
“I’m excited about the direction Dr. Toosi is taking — looking at the molecular effects of tAIH — as I believe this is the future of this work,” says Muir.
She envisions targeted therapy as the long-term goal. While tAIH is considered safe, pharmaceutical therapies that target molecules of interest could be a more effective treatment — sparing people from hypoxic treatments.
The potential implications of this area of research are vast. tAIH’s effect of enhancing plasticity could improve the lives of people with motor deficits beyond SCI.
“One of the most interesting things about [this work] is that it’s also being applied to other types of nervous system injuries. Researchers at USask and internationally are investigating whether tAIH enhances plasticity in people with multiple sclerosis (MS) or carpal tunnel [syndrome] and can improve their neural function,” says Muir.
Challenges faced
While promising, research on tAIH and SCI faces the same challenges that other neuroscientists face: the dazzling complexity and adaptability of the nervous system.
“Two people with identical lesions in their spinal cords [can have] very different functions,” says Muir. “This drives home the fact that we don’t fully understand the nervous system — not just how it works, but also how it develops, and how it reacts to injury.”
In the end, it’s the potential to improve lives that fuels the dedication of both Muir and Toosi to their research work. After years of investigating SCI and the recovery of function, the research team continues to move scientific understanding closer to a future where individuals with spinal cord injuries might be able to regain their independence and enjoy a better quality of life.
Emily Yau of Coquitlam, B.C., is a third-year veterinary student who worked as a summer research student in 2024. Her story is part of a series of articles written by WCVM summer research students.
Together, we will undertake the research the world needs. We invite you to join by supporting critical research at USask.
